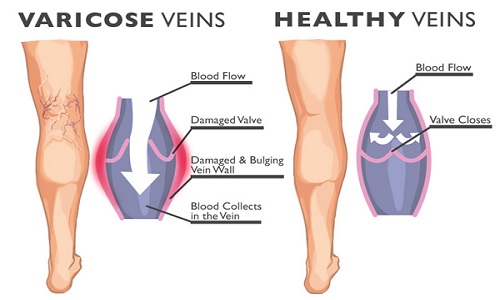
- Varicose veins develop when blood doesn’t flow properly through the veins in your legs. There are two main types of veins in your legs, superficial veins that lie under the skin and deep veins. The superficial veins include the long and short saphenous veins. The saphenous veins are connected to the deep veins inside your legs by perforator veins. When blood doesn’t flow properly from your superficial veins to your deep veins, pressure can build up. This results in blood collecting or pooling in your superficial veins. When this happens, the affected veins are called varicose veins.
- Varicose veins are very common – they affect up to a third of people.
SYMPTOMS OF VARICOSE VEINS:
Symptoms of varicose veins can vary. Some people don’t have any symptoms at all. If you do have symptoms, they may include:
- aching or discomfort in your legs
- itchy or restless legs
- swollen ankles
- lumps and blue or purple colouring under your skin.
Large varicose veins don’t always cause more discomfort than smaller varicose veins.
These symptoms may be caused by problems other than varicose veins. If you have any of these symptoms, see your GP for advice.
COMPLICATIONS OF VARICOSE VEINS:
Complications of varicose veins include the following.
- Thrombophlebitis – your superficial veins can become painful and reddened due to inflammation or a blockage in your veins.
- Bleeding – your varicose veins can bleed if you cut or bump your leg.
- Varicose eczema – your skin can become brown or purple. This is often permanent.
- Venous ulcers – you can get ulcers when fluid leaks out of the varicose vein into the surrounding tissue.
CAUSES OF VARICOSE VEINS:
If you have varicose veins, it’s thought that your vein walls are weak, and that this causes the valves in your veins to expand and separate, which damages them. Blood cannot travel up your veins as well or as easily as it should, and is more likely to pool.
You’re more likely to develop varicose veins:
- as you get older
- if you’re pregnant (because of the increased pressure on your veins)
- if you’re very overweight (also because of the increased pressure on your veins)
DIAGNOSIS OF VARICOSE VEINS:
Your GP will ask about your symptoms and examine you. He or she may also ask you about your medical history.
If your symptoms are severe or you have any complications, your GP may refer you to a vascular surgeon (a doctor who specialises in blood vessels).
Varicose veins are easy to see in your leg. However, to work out the position and extent of any valve damage, your doctor may perform the following tests.
- A Doppler test. This is an ultrasound technique that uses sound waves to produce an image of the inside of your leg. It will give your doctor information about the direction of blood flow in your vein and whether your valves are working properly.
- An ultrasound scan (duplex). This will allow your doctor to examine your deep veins in detail.
TREATMENT OF VARICOSE VEINS:
If your varicose veins don’t cause you any discomfort, you may decide not to have any treatment. If you do want treatment, your doctor will explain the options to you and help you decide which treatment is best for you.
SELF-HELP
Try not to stand for long periods of time as this may make your symptoms worse. Resting your legs up on a stool may ease any discomfort.
NON-SURGICAL TREATMENTS
Compression stockings can help the blood in your veins to flow up towards your heart. The stockings may relieve the swelling and aching in your legs, but it isn’t known if they prevent more varicose veins from developing.
VARICOSE VEIN SURGERY
Varicose vein surgery involves removing any superficial veins that have become varicose veins. The veins which are situated deep within your legs will take over the role of the damaged veins.
There are many types of operation. The operation you have will depend on which veins need treatment. The most common operation is ligation and stripping. This is where your surgeon ties off the faulty vein (ligation) to stop blood flowing through it and then removes it (stripping). You may have phlebectomy with ligation and stripping. This is used to remove the smaller surface veins that lie under your skin. Your surgeon will use hooks to pull out your varicose veins through small cuts in your leg.
Although many people won’t need any further treatment after surgery, it’s possible that the varicose veins can come back.
Sclerotherapy (liquid or foam)
This treatment involves injecting a chemical into your varicose veins. This will damage the veins and close them. Liquid sclerotherapy is often used to treat smaller varicose veins. For larger veins, foam sclerotherapy is used. Either a compression bandage will be put over the area after this procedure or you may be asked to wear compression stockings for up to four weeks.
Studies have shown that this treatment is effective at treating varicose veins in the short-term. However, the long-term benefits of this treatment aren’t yet known. The procedure also has serious potential complications (problems that occur during or after the procedure), such as a stroke or heart problems, and shouldn’t be performed if you have a previous history of DVT. It’s important to discuss the safety of ultrasound guided foam sclerotherapy with your doctor.
ENDOVENOUS LASER TREATMENT
Your surgeon will pass a fine laser inside your varicose vein. The laser heats the inside of your vein and causes damage to the vein wall. This causes the vein to close.
Radiofrequency ablation
Your surgeon will use a high frequency electrical current to heat the wall of your varicose vein. This damages the vein causing it to close.
Transilluminated powered phlebectomy
Transilluminated powered phlebectomy (TIPP) is a newer treatment and less is known about the long-term effectiveness of the treatment. Your surgeon will place a special light under your skin and remove the varicose vein by suction.
Your surgeon will explain your options to you and help you decide which treatment is best for you.
PREVENTION OF VARICOSE VEINS:
Although there are no scientifically proven ways to prevent varicose veins, the following suggestions may be useful.
- Don’t stand still for long periods of time.
- Take regular exercise, such as walking.
- Maintain a healthy weight.
- Wear properly fitted compression stockings to prevent your varicose veins from getting worse.


No comments:
Post a Comment